
Rectal Cancer - Management in the Modern Era
Rectal cancer is a cancer of the distal part of the large intestine. While colon cancer and rectal cancer are often referred to as "colorectal cancer", the management of each is quite unique.
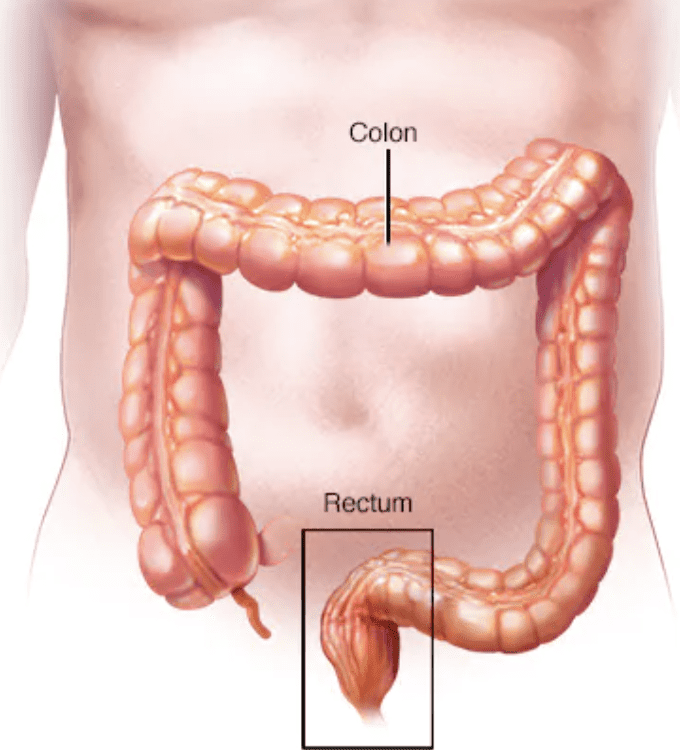
The anatomoic location of the rectum in the pelvis, where it sits close to other important organs such as the vagina and uterus in women and prostate and seminal vesicles in men as well as the sacral bone and anal sphincter muscles creates unique challenges in the management of this disease.
The complex management of rectal cancer depends on the stage.
Initial workup includes a CT of the Chest, Abdomen and Pelvis to evaluate for possible spread to the lungs, liver, or orther abdominal organs. A MRI of the pelvis provides more detailed assessment of the depth of tumor penetration through the wall of the rectum and presence of positive lymph nodes near the rectum. Once the stage of the tumor is determined, treatment decisions may be made by a multidisciplinary team. Evidence shows that cancers managed by such teams lead by high volume surgeons offer optimal outcomes. At Cedars Sinai, I lead the multidisciplinary tumo board which meets regularly to review and provide input on complex cases.
Stage I rectal cancer can be treated with surgery alone.
While most rectal cancers require resection of the rectum, some Stage I cancers with good prognostic features may be managed with a local excision through the rectum, removing the tumor without scars. This type of surgery is called TAMIS (Transanal minimally invasive surgery). My experience in transanal endoscopic surgery allows me to provide this option for many patients to achieve cure without sacrificing cancer results.
Stage II and III rectal cancers are frequently treated with chemoradiation to shrink and downstage the tumor prior to surgery.
Many patients then need further chemotherapy after surgery. Total neoadjuvant therapy is a modern chemoradiation approach used to provide all the chemotherapy and radiation before surgery and with this approach, over 30% of rectal cancers can achieve a complete response (destruction of all cancer cells) and hence excellent prognosis for the patient.
Surgery for Stage II and III rectal cancer is called a TME (total mesorectal excision). In this operation, the rectum and lymph nodes that drain the rectum are removed in one piece and the colon may be connected to the low rectum or anus. Cancers that involve the anal sphincter muscles often require removal of the anus and a permanent colostomy. In traditional practice, any cancer in the low rectum requires a permanent colostomy. However, in my experience and practice, rectal cancers in the low rectum with minimal involvement of the anal sphincter downstaged with chemoradiation may be managed with a reconstructive sphincter preserving operation without a permanent stoma. This decision requires a detailed multidisciplinary case review, thorough examination, and good imaging review to assure that the cancer can be removed with a negative margin to avoid sacrificing cancer outcomes.
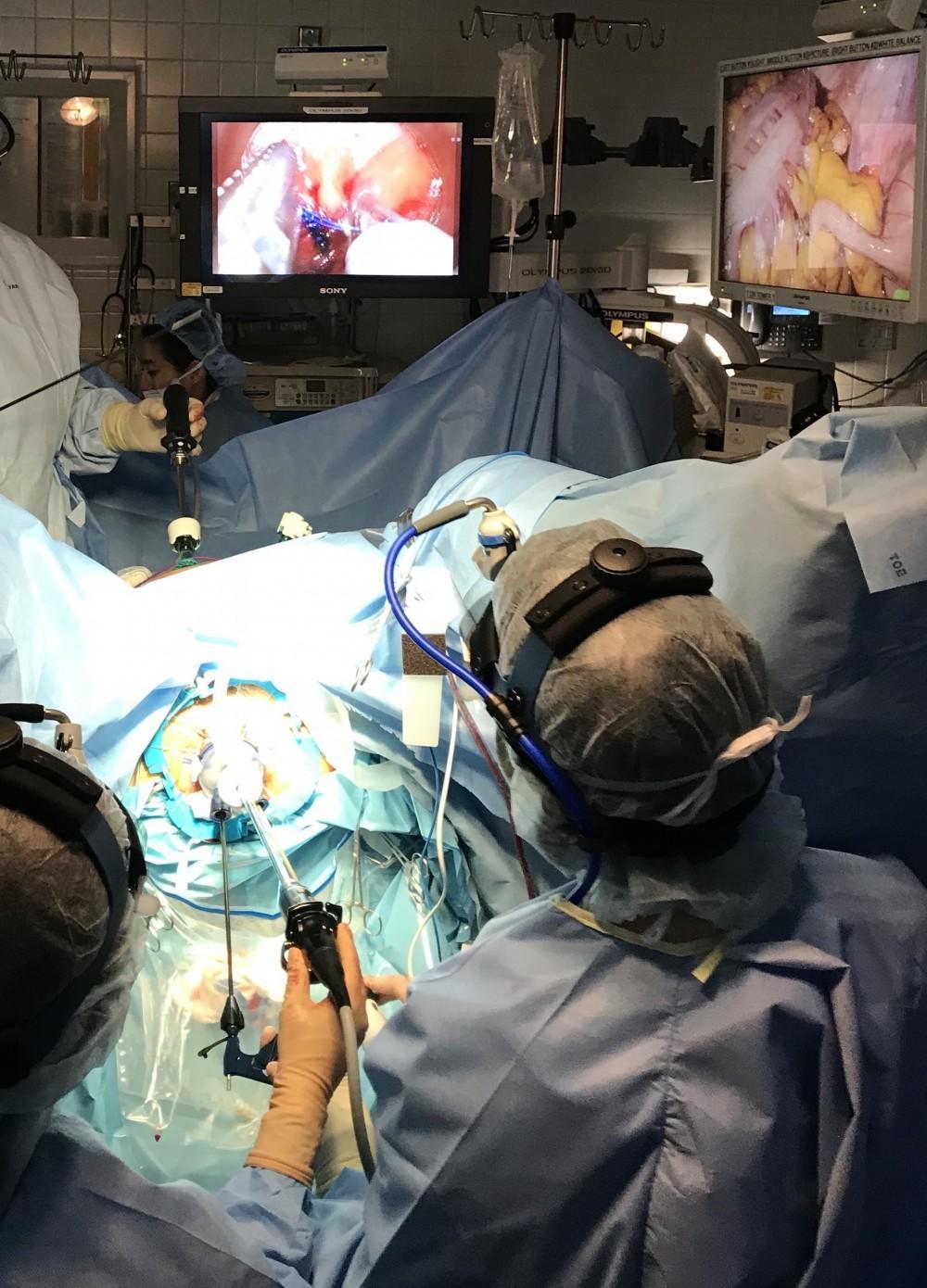
My experience as a pioneer in both robotic and transanal total mesorectal excision (taTME) allow me to provide optimal surgical results for patients facing rectal cancer. As a leader in taTME surgery and research, the ability to work bottom up to secure a negative margin on a low rectal cancer allows me to offer this unique strategy called an intersphincteric resection (ISR) for patients who may otherwise not be candidates for sphincter preservation.
Watch & Wait
Another modern approach to rectal cancer is the "watch and wait" or "nonoperative mangement" approach. Patients interested in a non-operative strategy must qualify based on several criteria and be committed to a stringent surveillance plan. After chemoradiation or total neoadjuvant therapy, a repeat MRI and flexible sigmoidoscopy are performed to assess tumor response. Patients who have a complete clinical response (resolution of all visible tumor on scope and MRI) may be managed without surgery and intensive surveillance with repeat scope, blood work and MRI every 3-6 months. As long as there is no sign of cancer, monitoring without surgery continues. With this approach, in about 30% of patients, the cancer will come back and surgery will be needed. This protocol is new and in the early stages of development and patients must understand these risks and be committed to frequent followup and scans to participate.
Immunotherapy
Another exciting area in rectal cancer management is in immunotherapy. Dostarlimab, a immunotherapy drug in the class of PD-1 Blocking therapies recently made headlines when authors published results of 12 patients with rectal cancer treated with this drug, all of whom had a complete response with no evidence of tumor on any diagnostic test. While these results are very exciting, participants all had a specific tumor mutation making them MMR-deficient or microsatelite unstable cancers - a class of cancers long known to have excellent response to immunotherapy drugs. Patients with MMR-D rectal cancer may be offered neoadjuvant immunotherapy, with consideration of watch and wait in clinical trials.
Circulating Tumor DNA
On the surveillance front, circulating tumor DNA is paving the way in which we monitor patients for cancer recurrence. Traditionally, the CEA blood test was used to monitor the blood for cancer recurrence after treatment and surgery. However, many cancers do not produce CEA, making this test a useless assay for early detection of cancer recurrence. ctDNA uses specific DNA blood testing to detect small cancer DNA in the blood stream to provide an early sign that the cancer may be coming back. Our preliminary research on the use of ctDNA has shown very promising results and I believe in the use of this tool to monitor my patients after surgery or treatment for rectal cancer.
With so many new treatments and surgical approaches on the horizon, the outlook for patients with rectal cancer is improving. I am excited to be on the cutting edge providing patients with the most novel treatment approaches to assure optimal outcomes. Working in collaboration with the best oncologists, radiation oncologists, radiologists, geneticists, nurses, and technicians at Cedars Sinai Medical Center and the Samuel Oschin Comprehensive Cancer Institute in Los Angeles allows me to provide the best possible care for my patients.


.svg)




