
A Letter to Patients With Crohn's Disease Considering Surgery
Dear patient,
If you have Crohn’s disease, you are no stranger to intestinal troubles. Chances are, you have been poked, scoped and imaged many times during your Crohn’s journey. As one of the most challenging gut conditions, Crohn’s can affect individuals quite differently. While some patients have very minimal disease that’s easily controlled with medication, others have suffered unstoppable diarrhea, bloating, recurrent blockages or a fistula. If you are one of the latter, you have probably asked yourself, “Why me???”.
If you have been referred to me for colorectal surgery, or if your independent search has led you my way, I would like you to know, that I will do everything in my power to make this process as easy as can be. Of course, you must be terrified, especially because you have already been through so much and there is no cure for your disease. You may be wondering if there is a diet or different medical option that may help. You may feel like your current state of poor health is better than going under the knife. You may be thinking, “How can my body even handle surgery? I’m so malnourished!”. You may fear the complications of surgery, or the possibility of an ileostomy may deter you. While surgery for Crohn’s is no easy feat, the expertise of your surgeon is key in getting you through the process.
The most common operation for Crohn’s is a limited ileocolic resection, one of the easier surgeries to bounce back from. Others, however, may need multiple surgeries in stages. Some may need a total colectomy with the option of a J-pouch or an ostomy operation may be recommended.
Multimodal Approach
No matter which surgery you are considering, your surgeon’s expertise is very important. As a board-certified colorectal surgeon in Los Angeles, CA and expert in inflammatory bowel disease (IBD) surgery at Cedars Sinai, my holistic approach will assure there is no stone unturned to make sure you have a great outcome. Firstly, patients considering surgery with me will be assessed for malnutrition and referred to an IBD dietician for perioperative nutritional support. Many studies have shown that perioperative nutritional support is one of the most important measures in assuring improved outcomes in IBD surgery. In addition, I will encourage regular exercise in the months to weeks leading up to surgery. Even a brisk walk daily can reverse many risks of surgery in debilitated IBD patients. Candidates will also be referred to our exercise prehabilitation program for additional support. For patients on steroids like prednisone, we will taper you off, or down to the lowest possible dose to minimize steroid complications during and after surgery. The literature has shown no adverse impact from other biologic or immunomodulator medications so if you are taking other drugs, these won’t affect your surgical outcomes. Patients needing an ostomy will meet with our expert stoma nurse, Jenn, before and after surgery. Patients rave about Jenn’s bedside manner, and she can troubleshoot the most pesty stomas in town. Jenn is an integral part of our team, and an asset to our practice.

Surgery
Now lets talk about the actual surgery. Everyone knows about minimally invasive or keyhole surgery, and most surgeons offer this to some extent. Unfortunately, many surgeons still do a limited portion of the surgery through a minimally invasive approach. Many surgeons rely on hand-assisted laparoscopy (HALS), where the surgeon’s hand is placed into the abdomen through a large wound, and the intestines are manipulated and detached by hand using visualization provided through a keyhole laparoscope. This approach is still called “minimally invasive” or “laparoscopic” but results in extensive tissue handling and trauma. Other surgeons may detach the intestine using small ports and a key-hole laparoscope, but still reconnect it through an open wound. This type of surgery, while better, than the old-fashioned open operation, carries many limitations, and while it is not maximally invasive, it sure isn’t minimally invasive.

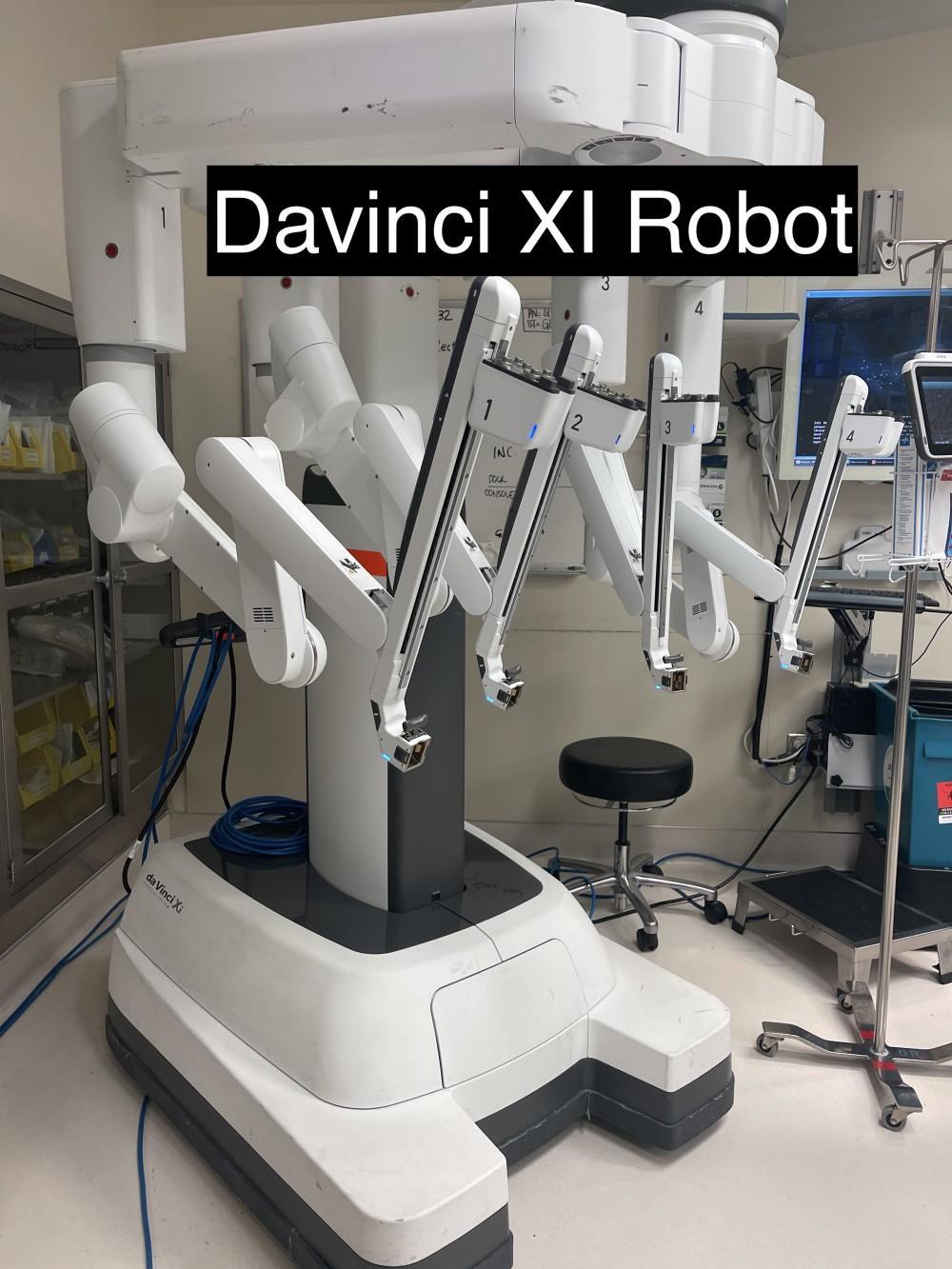
Minimally Invasive Approach
As an expert in robotic and fully minimally invasive (multiport or single port-laparoscopic) surgery and one of the pioneers in transanal Jpouch surgery, I vow to give my patients the minimally invasive outcomes I would want or hope for if I or my loved one was to go under the knife. With my minimal touch approach, incisions are as small as can be and uninvolved bowel is left untouched to minimize postoperative scar tissue and infertility complications. Intestines are cut and reconnected all under robotic or laparoscopic surgery. We have a magnified 3D view that provides superior visibility to assure a successful operation. I also use near-infrared imaging with a special dye called indocyanine green (ICG) to check the blood flow to the tissues before reconnection. This step makes sure there is no problems with blood flow that may risk gangrene or a leak at the intestinal connection site.
Pain Management
Now let’s talk about pain. Most individuals having surgery are worried about how much pain they will experience. Patients are also worried about taking narcotics and becoming addicted to opiates. Our enhanced recovery protocol has been published extensively and works wonders to improve postoperative pain. Using a combination of non-opiate pain medications given before surgery, as well as the nerve block (TAP block) I do during surgery, I have been able to significantly reduce pain scores and use of opiates in my patients after surgery.
While these points may seem like minutia, taken together, I have been able to see a dramatic improvement in patient outcomes after surgery. This means that patients experience less pain, take less pain medicine, leave the hospital sooner, and return to normal life earlier. These outcomes also translate to reduced scar tissue, bowel obstructions or blockages down the road, and fewer problems with scar-tissue induced infertility.
Once again, I thank you for entrusting me with your care. IBD patients are some of the most resilient individuals I have met and had the honor to help through my surgical expertise. I am honored to be a part of your journey.
With Love,


.svg)




